Opioids Unpacked
Researcher Todd Vanderah unravels the mysteries of pain in a journey marked by personal loss.

Todd Vanderah has dedicated his career to reducing pain in cancer patients through medication other than opioids.
/ UArizona Health Sciences photo
Todd Vanderah ’91 ’95 remembers the day he was remodeling a house with his dad, James, who complained of back pain. When his dad went to the doctor, the diagnosis was grim: Stage 3 lung cancer had metastasized to the bone. Vanderah’s father was only 58 years old when he died.
Vanderah says he was powerless to help his father, who was in unbearable pain. His frustration grew when the prescribed opioids caused even more problems.
“The doses of opiates were huge,” says Vanderah, who now is head of the pharmacology department and director of the Comprehensive Pain and Addiction Center (CPAC) at UArizona Health Sciences.
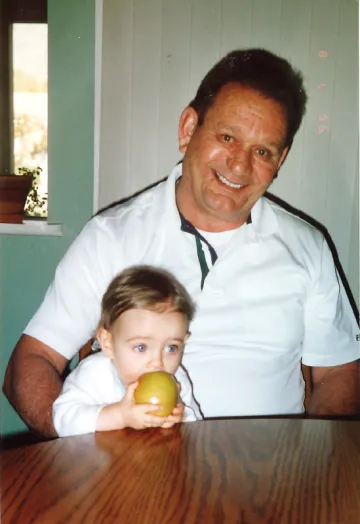
Todd Vanderah with his father, James, who died of lung cancer at age 58.
/ UArizona Health Sciences photo
“He was an absolute zombie, and the constipation was bad. He couldn’t enjoy the last parts of his life.”
Vanderah learned that opiates do little to inhibit pain; instead, they mask it, he says. “They take your brain offline, so you don’t think about the pain as much.”
James Vanderah’s battle with cancer ended one evening in 2004 after he took a high dose of opioids to get some rest. He never woke up — succumbing to respiratory depression, a deadly opioid side effect.
The experience changed Todd Vanderah’s understanding of cancer treatment, and he has made it his mission to discover non-opioid pain treatments for managing pain in cancer patients.
The makings of an epidemic
But Vanderah’s passion for pain research began even before his father’s death. “My interest in pain research started because I wanted to understand opiates. I still do,” he says.
He studied molecular and cellular biology as an undergrad in the UArizona College of Science. He went on to earn a Ph.D. from the College of Medicine – Tucson, where he conducted research with former professor Henry Yamamura and Frank Porreca, a UArizona professor of pharmacology and the associate research director of CPAC.
“Vanderah was a dedicated student researcher,” Porreca says. “When Todd joined the laboratory, he played a key part in understanding the role of endogenous opioid peptides and their receptors in brain circuits.”
Vanderah’s research showed that non-opioid molecules are less likely than opioids to cause respiratory depression or addiction. That’s why, in 1995, Vanderah was skeptical about the Food and Drug Administration’s approval of OxyContin to treat chronic pain.
FDA experts believed the extended-release formulation of oxycodone would reduce the potential for addiction — that it would be absorbed slowly, without creating an addictive “high.”
Vanderah did not agree.
“I kept saying, ‘Opiates, if overused or misused, are dangerous. We must come up with other ways to help people with chronic pain. This is not good.’” But it didn’t matter, he says. “There was a big wave when OxyContin came along — opiates were pushed forward and everything else aside.”
It wasn’t until years later that the FDA realized Vanderah and others like him were right. Reports of prescription drug overdoses and deaths began to rise in the early 2000s, and OxyContin was at the center of the problem. The number of people admitting to using OxyContin for nonmedical purposes skyrocketed, from approximately 400,000 in 1999 to 2.8 million in 2003.
Since 1999, more than 1 million people in the U.S. have died from drug overdoses. Opioid-related deaths account for more of the total than any other cause.
In 2010, Purdue Pharma stopped selling the original form of OxyContin to pharmacies after the FDA approved a reformulated version designed to make the drug more difficult to misuse. But the damage was already done.
Why are opioids dangerous?
According to Vanderah, opioids trigger the brain’s reward center. They release dopamine and endorphins, boosting feelings of well-being while muting sensations of pain and anxiety. Most people who take opioids develop a tolerance and must take higher doses to feel good or get pain relief.
“We investigated opioid tolerance and found that, when opioids are present, the brainstem can’t turn on the pathways that promote pain,” Vanderah says, citing it as one of the most significant findings to come out of his laboratory.
Without pain, he explains, we wouldn’t survive. Sensations of pain signal people to protect themselves from harm and even death.
“Physiologically, if you shut off the sensation of pain for too long, your body tries to figure out how to overcome that,” Vanderah says. “Our preclinical findings suggest that opioid tolerance is the body trying to make pain to overcome the opioid.”

Todd Vanderah still builds homes after learning the craft from his father. Inspired by his father, and forever changed by his experience caring for him during his father’s cancer treatments, Vanderah’s present research asks whether cannabinoids might replace opioids in helping cancer patients endure pain.
/ UArizona Health Sciences photo
Finding a better way
Ten years after his father’s death, Vanderah faced another personal loss. He was golfing with his mentor, Yamamura, who complained of back pain as Vanderah’s father had. He, too, was diagnosed with lung cancer.
After Yamamura’s death, Vanderah was even more committed to researching cancer pain. And he began researching how opioids affect metastatic cancer at the cellular level. His preclinical research projects have led him to believe that chronic opioid use increases pain and enhances bone loss in metastatic cancer models.
At the same time, he began taking a closer look at cannabinoids — compounds found in the Cannabis sativa plant. When he discovered an Israeli research paper about cannabinoids for treating osteoporosis, he remembers thinking, “This is it!”
“I realized that the cells of the bone actually have CB2 receptors, one of the cannabinoid receptors.”
Now, the early results from his research on using unique, structured cannabinoids to inhibit pain are promising. And he is studying the effects of an FDA-approved cannabinoid on pain and bone loss in cancer patients.
“The goal is to help metastatic cancer patients reduce pain and bone loss — and possibly decrease the proliferation of the tumor,” Vanderah says.
“I’ve made progress in treating metastatic cancer pain with something other than opiates.”
