Simulation for the Future

The future of modern health care simulation and training can be summed up in two words: artificial intelligence. Technological advancements have dramatically changed the way simulation is used to teach and train aspiring health care providers, and AI will be no exception. As AI continues to rapidly evolve and become a part of everyday life, its application in health care simulation will also become commonplace, just as other technologies have become standard in recent years.
The Arizona Simulation Technology and Education Center (ASTEC) is adapting to the changing health care landscape to train the next generation of providers. Allan Hamilton, MD, ASTEC’s executive director, discusses how health care simulation has evolved, how AI can best be implemented, and what is next for simulation in educating the next generation of health care professionals.
Educating with Artificial Intelligence
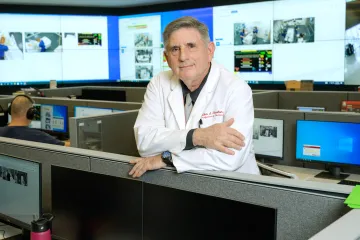
Allan Hamilton, Arizona Simulation Technology and Education Center executive director
Hamilton: We have more technology available now than ever before. We use augmented reality, mixed reality, immersive reality and high-quality haptics. There really is this profusion of technology which may, to some extent, improve our educational outcomes. But I look forward to fine-tuning simulation with AI.
From an education and training perspective, it is hard now for one of our students to be able to intercept and see everything from start to finish for a particular patient. That is where medical simulation is really a strength, because we can go back and teach what may have been missed in the clinical experience for a student. If a student didn’t see a heart attack case when they were in the unit, we can simulate one.
So, in a sense it has evolved to a point where it allows us to standardize things and consider problems of patient continuity. For us at ASTEC, our education gets divided into procedural-based training, scenario-based training, and then interprofessional education and leadership.
Every single problem that we’ve had in medicine is only getting worse. Shortages of personnel are continuing, patients are being moved through the system faster and faster to maximize profitability, and there is much more outpatient care than we ever had before. The breakup of continuity in patient care doesn’t provide enough range for us to teach students. Back when I was training, I might see 100 cases of certain types of patients. Now, they might not see any, or only a couple, of a certain patient. Medical simulation allows us to create those patients and those scenarios.
We are really starting to look at, “How do we turn out the ideal health care provider?” — whether that is a doctor, nurse practitioner, nurse anesthetist, physical therapist or nurse-midwife. More and more of what we’re looking at is, “What are the things that we can do in a sim lab where we have a lot more control?” We are looking to see where we can take the guesswork out, where we can take the subjectivity out.
This allows us to better calibrate the education process and vary it from individual to individual. We want simulation to work on everything, but one student might be very gifted with their hands, and another might be gifted with their recall. As trainers, it is important we make that distinction, because we have different tools that help students work on different things.
The last part of this is that the processes we can simulate allow for the patient to have the absolute safest experience. Our goal at ASTEC is to look toward a world in which no one suffers an avoidable medical adverse event. That’s our goal, and to achieve that, we have to stay at the top of our game now and in the future.
